Overview
-
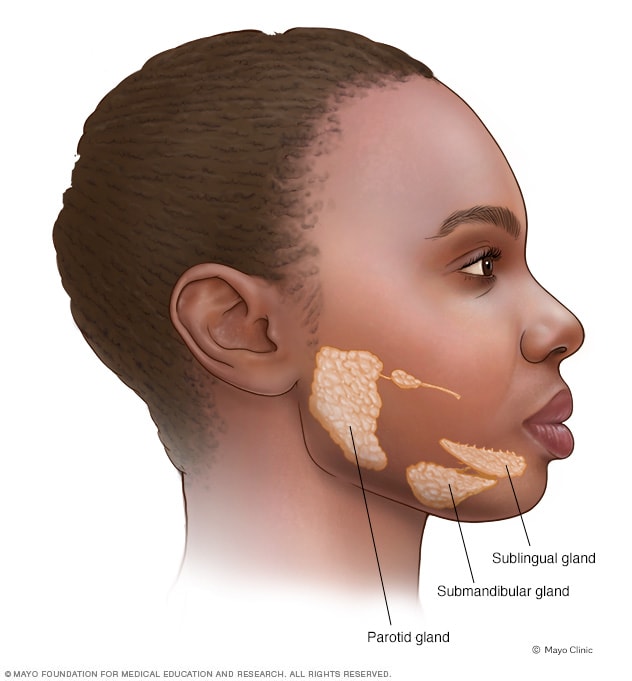
Salivary glands
Mumps is a viral infection that primarily affects saliva-producing (salivary) glands that are located near your ears. Mumps can cause swelling in one or both of these glands.
Mumps was common in the United States until mumps vaccination became routine. Since then, the number of cases has dropped dramatically.
However, mumps outbreaks still occur in the United States, and the number of cases has crept up in recent years. These outbreaks generally affect people who aren't vaccinated, and occur in close-contact settings such as schools or college campuses.
Complications of mumps, such as hearing loss, are potentially serious but rare. There's no specific treatment for mumps.
Symptoms
-
Mumps
Some people infected with the mumps virus have either no signs or symptoms or very mild ones. When signs and symptoms do develop, they usually appear about two to three weeks after exposure to the virus.
The primary sign of mumps is swollen salivary glands that cause the cheeks to puff out. Other signs and symptoms may include:
- Pain in the swollen salivary glands on one or both sides of your face
- Pain while chewing or swallowing
- Fever
- Headache
- Muscle aches
- Weakness and fatigue
- Loss of appetite
When to see a doctor
See your doctor if you or your child has signs and symptoms of mumps. Mumps is highly contagious for about nine days after symptoms appear. Tell your doctor's office before you go in that you suspect mumps so arrangements can be made to avoid spreading the virus to others in the waiting room.
In the meantime:
- Rest as much as possible
- Try to ease symptoms with cold compresses and over-the-counter pain relievers such as ibuprofen (Advil, Motrin IB, others) and acetaminophen (Tylenol, others)
Mumps has become uncommon, so it's possible that another condition is causing your signs and symptoms. Swollen salivary glands and a fever could indicate:
- A blocked salivary gland
- A different viral infection
Causes
Mumps is caused by a virus that spreads easily from person to person through infected saliva. If you're not immune, you can contract mumps by breathing in saliva droplets from an infected person who has just sneezed or coughed. You can also contract mumps from sharing utensils or cups with someone who has mumps.
Complications
Complications of mumps are rare, but some are potentially serious.
Most mumps complications involve inflammation and swelling in some part of the body, such as:
- Testicles. This condition, known as orchitis, causes one or both testicles to swell in males who've reached puberty. Orchitis is painful, but it rarely leads to the inability to father a child (sterility).
- Brain. Viral infections such as mumps can lead to inflammation of the brain (encephalitis). Encephalitis can cause neurological problems and become life-threatening.
- Membranes and fluid around the brain and spinal cord. This condition, known as meningitis, can occur if the mumps virus spreads through your bloodstream to infect your central nervous system.
- Pancreas. The signs and symptoms of this condition, known as pancreatitis, include pain in the upper abdomen, nausea and vomiting.
Other complications of mumps include:
- Hearing loss. Hearing loss can occur in one or both ears. Although rare, the hearing loss is sometimes permanent.
- Heart problems. Rarely, mumps has been associated with abnormal heartbeat and diseases of the heart muscle.
- Miscarriage. Contracting mumps while you're pregnant, especially early in your pregnancy, may lead to miscarriage.
Prevention
The best way to prevent mumps is to be vaccinated against the disease. Most people have immunity to mumps once they're fully vaccinated.
The mumps vaccine is usually given as a combined measles-mumps-rubella (MMR) inoculation, which contains the safest and most effective form of each vaccine. Two doses of the MMR vaccine are recommended before a child enters school. Those vaccines should be given when the child is:
- Between the ages of 12 and 15 months
- Between the ages of 4 and 6 years
College students, international travelers and health care workers in particular are encouraged to make sure they've had two doses of the MMR vaccine. A single dose is not completely effective at preventing mumps.
A third dose of vaccine isn't routinely recommended. But your doctor might recommend a third dose if you are in an area that is experiencing an outbreak. A study of a recent mumps outbreak on a college campus showed that students who received a third dose of MMR vaccine had a much lower risk of contracting the disease.
Those who don't need the MMR vaccine
You don't need a vaccination if you:
- Had two doses of the MMR vaccine after 12 months of age
- Had one dose of MMR after 12 months of age and you're a preschool child or an adult who isn't at high risk of measles or mumps exposure
- Have blood tests that demonstrate your immunity to measles, mumps and rubella
- Were born before 1957 — most people in that age group were likely infected by the virus naturally and have immunity
Also, the vaccine isn't recommended for:
- People who have had a life-threatening allergic reaction to the antibiotic neomycin or any other component of the MMR vaccine
- Pregnant women or women who plan to get pregnant within the next four weeks
- People with severely compromised immune systems
Those who should get the MMR vaccine
You should get vaccinated if you don't fit the criteria listed above and if you:
- Are a nonpregnant woman of childbearing age
- Attend college or another postsecondary school
- Work in a hospital, medical facility, child care center or school
- Plan to travel overseas or take a cruise
Those who should wait to get the MMR vaccine
Consider waiting if:
- You're moderately or severely ill. Wait until you recover.
- You're pregnant. Wait until after you give birth.
Those who should check with their doctors
Talk to your doctor before getting vaccinated for mumps if you:
- Have cancer
- Have a blood disorder
- Have a disease that affects your immune system, such as HIV/AIDS
- Are being treated with drugs, such as steroids, that affect your immune system
- Have received another vaccine within the past four weeks
Side effects of the vaccine
The MMR vaccine is very safe and effective. Getting the MMR vaccine is much safer than getting mumps.
Most people experience no side effects from the vaccine. Some people experience a mild fever or rash or achy joints for a short time.
Rarely, children who get the MMR vaccine might experience a seizure caused by fever. But these seizures haven't been associated with any long-term problems.
Extensive reports — from the American Academy of Pediatrics, the Institute of Medicine and the Centers for Disease Control and Prevention — conclude that there's no link between the MMR vaccine and autism.
mumps
![mumps]() Reviewed by PatPew
on
tháng 12 09, 2018
Rating:
Reviewed by PatPew
on
tháng 12 09, 2018
Rating:


Không có nhận xét nào: